|
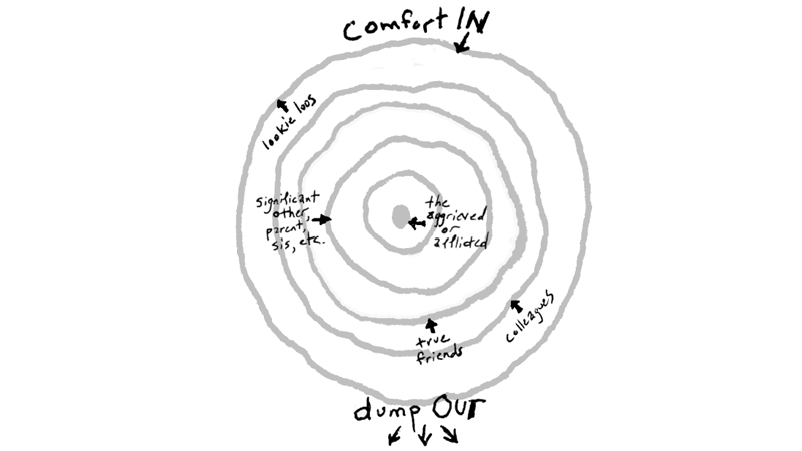
I recently had a conversation with a good friend who has a family member with a serious illness. She told me that close friends of the family had called her in distress about this family member, as if she was expected to comfort them! This made me remember an article I read recently about “ring theory.” I sent this article to my friend and suggested she send it to all of her friends and family. It’s important information about how to cope with friends and family who are dealing with a crisis or death. I think it is so necessary to understand, that I wanted to spread the word to all of you. (It’s also been called the circle of kvetching, for those who can relate to the Yiddish term). Here is the original article:
How Not to Say the Wrong Thing by Susan Silk and Barry Goldman Last year Elana Premack Sandler wrote this excellent explanatory article: Ring Theory Helps us Bring Comfort In by Elana Premack Sandler, LCSW, MPH A few years ago, psychologist Susan Silk and her friend Barry Goldman wrote a piece about a concept they called the “Ring Theory.” It’s a theory to help yourself know what to do in a crisis. If the crisis is happening to you, you’re in the center of the ring. If the crisis is not happening to you, you’re in one of the outer circles. Here are the basic tenets paraphrased from Silk and Goodman’s article:
The concept is simple: “comfort in, dump out.” I think disseminating this information will make the world a better place! It seems obvious when reading about the theory, but we have all likely been in the position of saying something similar that we later regretted. So please share this far and wide. As Susan Silk and Barry Goldman have said “And don’t worry. You’ll get your turn in the center ring. You can count on that.” As most of you know, I am a zealot for the overthrow of the healthcare “system”—since it is not adequately serving any of us. You might think overthrow is a bit of hyperbole, which I suppose it is, but I believe what we have now needs to be totally reworked, including how it is paid for. Putting patches on a sinking ship is too little too late.
An example of how badly this system—controlled by financial considerations—went off the rails has been in the news lately in Seattle. One of the major healthcare systems in our area underwent an expose by The Seattle Times; it seems the leadership of the neurosurgery department had lost its moral compass, and what was occurring was unethical and also illegal in some cases. Quality of care had been sacrificed for profit. A Lost Voice by Mike Baker Unfortunately, patients suffered poor outcomes and there was at least one death that likely could have been averted. Heads rolled, the head of the department lost both his job and his medical license, the CEO resigned, the state department of health investigated, JCAHO got involved (never a good thing), and major changes are underway. There are many fine doctors in this hospital system, and I was extremely gratified to learn that many in that department, many of whom I have worked with, very vigorously objected to the circumstances and some suffered repercussions (one just was awarded a large amount of money for being fired as a whistle blower!). The past chief executive of the system’s physician division confronted the leadership regarding the situation suggesting that action be taken. So why am I writing about this? For one, it confirms what I know to be true—most doctors are committed to doing what is right for their patients, do it well, and call out those who are acting counter to their principles. For another, when I initially read the articles in the paper about this investigation, I was screaming in my head “no, you need an advocate there!” A young woman lost her life, despite the fact that her father is a doctor and was present in the ICU urging those caring for her to do what was needed. His concerns went unheeded. Having someone who is not related to the patient serving as an advocate is invaluable. No one can think clearly when their child is struggling to breathe. As advocates, we have no qualms about raising a ruckus, confronting care givers, or going up the chain of command until we get what is needed, particularly when it is a life-threatening event. I would like to believe that if an advocate had been there this young woman would still be alive; I don’t really know if that is the case, but I do know that if I had been there, there would have been a lot more yelling and screaming going on. Sometimes that is the best thing an advocate can do. On that less than uplifting note, I do hope all of you had some rest and enjoyment over the holidays and are having a wonderful new year. Happy holidays to all of you!
This is a good time of year to look back at the year and do a survey of how well we are accomplishing our goals. I’ve been thinking about how to spread the word about healthcare advocacy, and this story struck me as a case in point. Recently a colleague and friend said to me that she had thought about calling me (as a healthcare advocate) when her son had been very ill. He was much better now, but the family had gone through a very difficult and scary time. I wondered what had made her hesitate while they were going through the health crisis. We met for lunch recently, and she told me the story. Here it is with many identifiers changed, and I’ve included my comments in italics where a healthcare advocate would have helped. This 22-year-old male’s past medical history is significant only for migraines, he has been active in sports and has been routinely healthy. He joined a fraternity in college and then moved into a house with friends where he began to have respiratory illnesses, and his health began to deteriorate. The house, which his mother describes as a dump (I thought that the house my son lived in his fourth year of university should be burned down when they moved out), was subsequently found to have black mold. He developed gastric ulcers that eventually bled and he was treated according to the appropriate protocol. In December of 2014, he called his mother during a particularly bad respiratory infection to “come get me”. She did, and he was found to have pneumonia. Due to his illness he had to take an extra semester to graduate, but he recovered at home with appropriate medical care and finished school in March of 2015. In October of 2015, his family noted that he was becoming more and more irritable, and he began to have more and more fatigue. (I should add here: this would not necessarily trigger a call to an advocate, but it would have been a good time for him to see his primary care doctor). Within 2 months he was sleeping more and more and eating less and less (again, see your doctor! This is not normal!). In January of 2016 he noticed blood in his urine. Was this a urinary tract infection? He saw a urologist, who also ordered a CAT scan, which was normal. The possibility that he had passed a kidney stone was considered, although the symptoms were not particularly characteristic for that, and my friend’s son did not think that it was likely. A week later his nausea, irritability, and fatigue had markedly increased. He saw a nephrologist at his medical clinic, who wondered if it was a virus. A creatinine was checked (this measures kidney function) and it was found to be 3.5 (abnormally high, especially for a young person). He was scheduled to have a scope of his bladder, but that was cancelled due to respiratory symptoms (asthma?). The next day, when he saw his urologist his creatinine was 5.5 (even worse! And rapidly worsening!) It was clear that something was going on that needed to be addressed urgently, and he was admitted to the hospital—and put on the oncology floor! Here is the first point where a healthcare advocate would have been helpful. The family felt lost in space. And he was on an oncology floor! An advocate could have helped with the communication between the medical team and the family, and explained that this did not mean he had cancer. At a time like this, someone who can keep track of all the pieces of information and relay them calmly to a very distressed patient and family can be priceless. He proceeded quickly to a diagnostic workup that led to the diagnosis of a rare autoimmune syndrome that attacks the kidneys. As a kidney biopsy confirmed this, his creatinine climbed close to 7, and his blood pressure increased. The doctors immediately began treatment with plasmapharesis (a method of removing blood from the body, separating the components, and reinfusing the cells but not the plasma--a way of getting rid of unwanted antibodies). They also treated him with prednisone, as well as an oral chemotherapeutic agent. He was told that 50% of his kidney tissue had been affected by the immune complexes. He believed, wrongly, that he was destined for a kidney transplant, and soon. Next place for an advocate to intervene: not all medical providers communicate well with patients, and making sure the patient and family have a realistic idea of what could lie ahead is important. The emotional distress that this misinformation caused was significant, and entirely unnecessary. He continued to have daily plasmapharesis for 4 weeks; his hospital stay was complicated by the development of a blood clot in his arm that required IV anticoagulation (overtreatment led to him bleeding from everywhere but dissolved the clot very rapidly), and a bout of hospital acquired pneumonia after about 2 weeks was treated with IV and oral antibiotics. One of his doctors took his pathology slides to a conference because it was so unusual. He was discharged after a 4-week hospital stay on 20 different medications. His creatinine is now around 1.5. What went well?
A healthcare advocate would have been able to work with the system and the patient to be sure he had some mental health consultation during the hospital stay. In addition, the family needed some support, and this also could have been facilitated. In addition, if the nephrologist is going to change weekly, the healthcare advocate can be the continuity to be sure all sides are hearing each other. Now: He is recovering at home, rides his motorcycle, and doing much better. He is off of chemo and has weaned down his prednisone. He has gotten much feistier (he doesn’t want his mom going to doctor appointments with him). But he went through a significant period of depression, and was even suicidal. He is on an antidepressant, which helps. He still feels under the influence of “chemo brain”, but this is slowly improving. And he is experiencing what sounds to me like PTSD. A healthcare advocate would stay involved after discharge from the hospital, and perhaps could have hastened treatment for the depression, as well as help find resources to treat PTSD. As my friend said, a healthcare advocate is like a SWAT team that can swoop in and make sure everything that needs attention gets attention. My friend’s son had a fairly rapid diagnosis, good medical care, and is doing much better. Even so, the journey could have been so much less painful, scary, and a much smoother ride with an advocate. A healthy new year to all! Dealing with serious illness and hospitalization can be scary, demoralizing, confusing, painful, unpredictable.
Your father is not his disease. Your mother is not her “medication options.” It's easy to get overwhelmed when people you love are sick and all you want is to help them. You're sailing to a new world where some of the landmarks seem familiar and others disappear. As a healthcare advocate, my job is to steer you to dry land and clarify your situation, to create a safe harbor where you can focus on yourself and your family. I get questions answered and stand up for you, stand in for you, stand beside you. You have a doctor at your side whose sole job it is to create and implement a plan so you can get the best possible care for who you are, with your specific health needs. That's what I do: advocate for you when medical care takes over. With a healthcare advocate: -You never need to undergo a treatment without understanding what it is, why it's needed, and what the alternatives are. -You have someone to communicate with your care team when you are feeling uncomfortable, uncared for, or unheard. -Your advocate can translate medical-ese into English, and statistics into solutions. When the world of diagnoses and hospitals and prescriptions and procedures overwhelms your life, you need someone to make sure that when the doctor leaves the room, you know the next steps. You need Healthcare Advocacy Partners. |
AuthorDr. Sima Kahn muses on being a healthcare advocate, the troubles with our healthcare system, and how to advocate for ourselves. Archives
August 2021
Categories
All
|

 RSS Feed
RSS Feed